Quest Enterprise ServicesTM (QESTM)
Provider Claims Insights
Optimize Provider Network Performance With Actionable Provider Insights
Build, Manage, Expand and Optimize Your Provider Network with Quest Enterprise Services Provider Claims Insights
Build, manage, expand, and refine your provider network effortlessly with Quest Enterprise Services Provider Claims Insights. Our all-in-one solution brings together foundational network adequacy analysis with additional reliable provider data, enabling you to go beyond traditional provider network management. Quest Enterprise Services Provider Claims Insights is not just a tool, it’s a catalyst for change—innovating and optimizing your provider network.
EFFICIENTLY FILL NETWORK GAPS
Identify Active, High-Performing Providers

ACCELERATE SPEED TO MARKET
Additional Data Insights to Streamline Network Builds and Expansion

OPTIMIZE YOUR PROVIDER NETWORK
Actionable Data Insights to Refine the Network
Enhancing Data To Drive Success
Enhance the performance and effectiveness of your provider network with Quest Enterprise Services Provider Claims Insights. Our comprehensive platform equips you with the tools and insights needed to make informed decisions in today’s evolving healthcare landscape.
Actionable Provider Insights: Uncover valuable data-driven insights to optimize your provider network. Identify high-performing providers, address areas for improvement, and enhance the quality of care, all while reducing costs.
Streamlined Network Building: Build compliant and competitive provider networks that meet your specific requirements. Leverage our comprehensive data on provider specialties, payer affiliations, and performance metrics to select the best-fit providers for your network.
Efficient Network Management: Simplify the management of your provider network with our intuitive platform. Streamline workflows, automate processes, and see information at a glance, saving time and resources.
Compliance Assurance: Stay compliant with industry regulations using our built-in compliance checks. Keep your provider network up to date with evolving standards, avoiding penalties or disruptions to your operations.
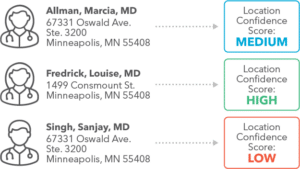
Making it Easier to Identify Practitioner Locations
Whether you’re filling network gaps, building a network, expanding your footprint, or optimizing your network, the last thing you want is for the provider to be listed at the wrong location. Quest Enterprise Services Provider Claims Insights with Machine Learning surpasses standard public data sets by integrating continuously updated proprietary data and provider attestations. We provide you with more reliable and trustworthy results about practitioner locations.
Practitioner at Location Confidence Scores
With our exclusive Practitioner at Location Confidence Scores, you can effortlessly identify the right provider location combination right from the start. By easily recognizing and avoiding locations where providers are not, you eliminate the need for future network modifications, ensuring a more streamlined and efficient network.
Enriching Provider Performance Insights
We understand the need for more extensive data to efficiently manage provider networks. With Quest Enterprise Services Provider Claims Insights, we take it a step further.
Gain access to additional provider performance measures that have been seamlessly integrated into Quest Enterprise Services Provider Network, Prospect, and Market files. These insights provide you with valuable information on provider capabilities and performance, enabling you to make more informed and strategic decisions about your network.
Provider Claims Activity
Is the provider active? In which line of business? Identify which providers are active and generating claims, and which providers are ghosts.
GHOST
No Patients
PERIPHERAL
Bottom 25% of patient volume
STANDARD
Middle 50% of patient volume
CORE
Top 25% of patient volume
Top Conditions & Procedures
What is the Provider’s Expertise? Top conditions and top procedures allow you to examine the provider’s full range of expertise beyond their general specialty.

Efficiency & Effectiveness Scores
Does the provider offer high-quality and cost-effective services? Discover which doctors provide excellent services at affordable prices and which do not.
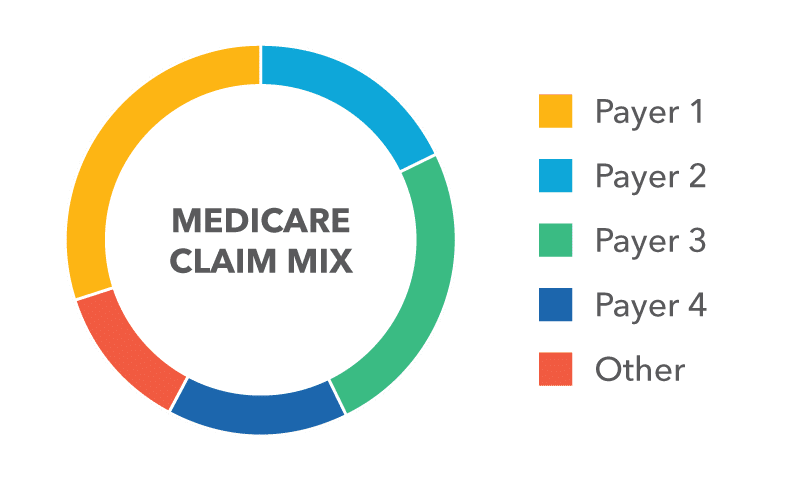
Payer Mix
Which payer does the provider work with? Insight into which providers are participating in competitor networks.
Practitioner at Location Confidence Levels
Want to know which provider location is the right one? Find out where they’re most likely to be practicing with confidence.
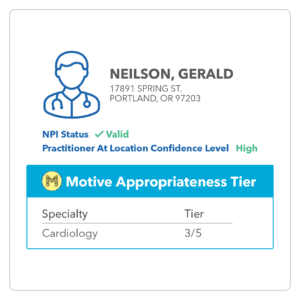
Clinical Appropriateness Measures Insights
Incorporating Motive Practicing Wisely Appropriateness Measures elevates your assessment of physician quality by emphasizing their adherence to clinical guidelines across 18 specialty care areas, from Cardiothoracic Surgery to Primary Care. This advanced analytical approach enhances your capability to create trusted networks aligned with the pinnacle of medical excellence.
Eliminating Ghost Providers
Ghost providers can cause financial setbacks and damage the credibility of your provider network. Eliza Hoffman, Vice President of the Regional Payer Segment at Quest Analytics, shares how Quest Enterprise Services Provider Claims Insights helps you identify ghost providers.
EXPERIENCE UNPARALLELED RETURN ON YOUR INVESTMENT
Save Time and Increase Efficiency
Accelerate Gap Filling: Identify the Right Providers, Right Away
Identifying the right providers to fill network gaps can be a time-consuming process, but not anymore. With Quest Enterprise Services Provider Claims Insights, we’ve streamlined the gap-filling process. Our detailed data insights enable you to quickly identify providers who meet your network requirements and avoid those who don’t.
Stand Out in the Market
Network Build: Enriched Data to Streamline Your Launch
Building a provider network that sets you apart from the competition is made easy with our enriched data insights. Easily identify and recruit top-tier providers who align with your organization’s goals and preferences. Create a network that meets the unique needs of your potential demographic and delivers exceptional care.
Meet the Needs of Your Members
Network Expansion: Gain Valuable Insights for Strategic Growth
Expanding your network is about cultivating a comprehensive network with top-quality services and a commitment to patient satisfaction. By carefully selecting providers based on membership requirements and the competitive landscape, you can meet your members’ medical needs and exceed expectations.
Improve Network Quality While Reducing Costs
Network Optimization: Curate and Refine Your Network
Enhance network quality and reduce costs by strategically optimizing your network. Explore different scenarios and visualize the impact of refining your network during the transition to value-based contracts. Uncover valuable insights to ensure your network is ready for the challenges of tomorrow.
Get Started with
Provider Claims Insights
Quest Enterprise Services Provider Claims Insights helps you improve the value of your provider network by ensuring it is adequate, accurate and active! Schedule a complimentary strategy session today to learn more.