Additionally, Quest Enterprise Services (QES) helps you respond confidently to accreditation agency requests, such as NCQA and URAC, with the ability to demonstrate an ongoing process for improvement and provide a real-time view of your network’s performance over time for primary care, behavioral healthcare, specialty care practitioners, facilities and more.
- Who We Help
Proven Provider Network Management
Quest AnalyticsTM brings you unrivaled provider network management solutions and services for healthcare provider networks, ensuring swift access to top-notch healthcare.
- How We Help
- For Providers
Provider Claims Insights
This state-of-the-art solution is your key to building and mastering competitive provider networks, placing you steps ahead in the healthcare landscape—all within an easy-to-use unified platform.
- About Us
- We Are HiringAbout UsEvents We Are A Part Of
We're Hiring
We’re Hiring. If You’re Looking To Use Your Talents To Make A Difference In The Lives Of Healthcare Consumers – We Want To Hear From You.
- Resources
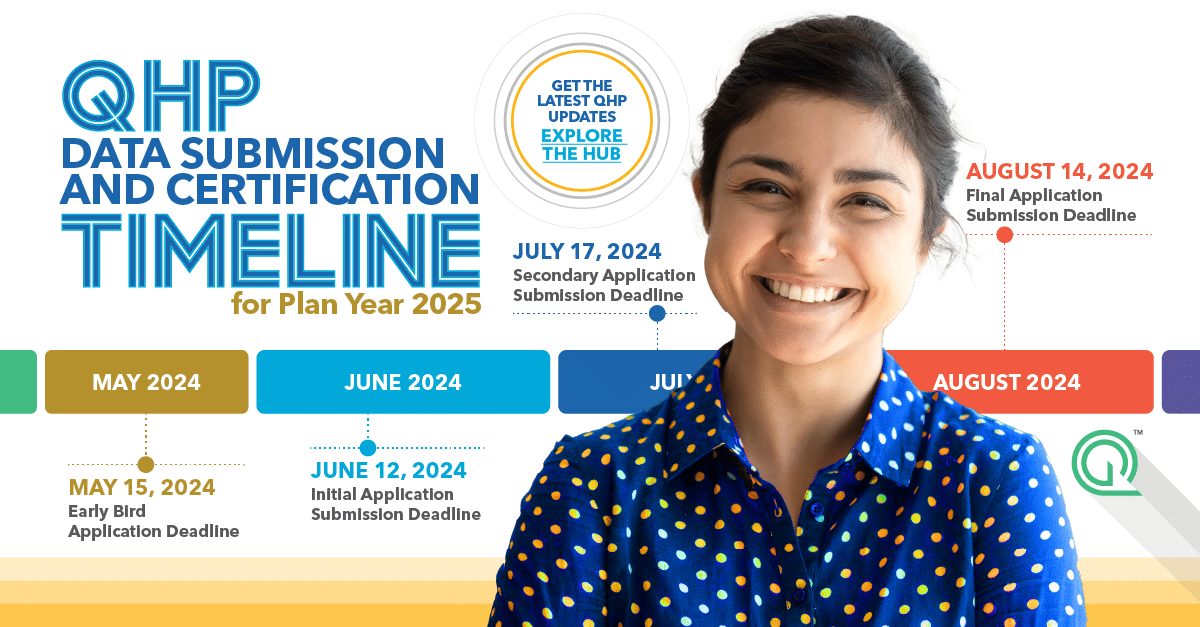
- Featured Resource HubsCase Studies8 Data Tips for Medicare Advantage Network Adequacy ReviewsYour provider network is your greatest strength, but a network with inaccurate data or ghost providers isn’t very efficient. Whether you’re fine-tuning your data for a Triennial Network Adequacy Review,...QHP Certification and Network Adequacy Review TimelineWho doesn’t love a good calendar? We know we do. Whether you’re deep into network adequacy updates or juggling deadlines left and right, we’ve got your back. Our handy calendar...Quest Analytics® Announces Strategic Integration Partnership with Motive Practicing WiselyOVERLAND PARK, KS, April 9, 2024 – Quest Analytics, LLC, the leader in provider network compliance and performance solutions, announced today a new integration partnership with Motive Practicing Wisely, the...The Hidden Costs of Not Having Accurate Provider Data & How to Solve ItYou’ve probably heard the buzz surrounding provider data accuracy, and you might be wondering just how important it is for your organization. Well, you’re not alone! We conducted a study...Understanding CMS Exception Requests for Network AdequacyRaise your hand if you’ve ever had difficulties meeting network adequacy criteria. Well, you’re not alone. Submitting an exception request for network adequacy involves multiple components, and we’re here to...
- Who We Help
Proven Provider Network Management
Quest AnalyticsTM brings you unrivaled provider network management solutions and services for healthcare provider networks, ensuring swift access to top-notch healthcare.
- How We Help
- For Providers
Provider Claims Insights
This state-of-the-art solution is your key to building and mastering competitive provider networks, placing you steps ahead in the healthcare landscape—all within an easy-to-use unified platform.
- About Us
- We Are HiringAbout UsEvents We Are A Part Of
We're Hiring
We’re Hiring. If You’re Looking To Use Your Talents To Make A Difference In The Lives Of Healthcare Consumers – We Want To Hear From You.
- Resources
- Featured Resource HubsCase Studies8 Data Tips for Medicare Advantage Network Adequacy ReviewsYour provider network is your greatest strength, but a network with inaccurate data or ghost providers isn’t very efficient. Whether you’re fine-tuning your data for a Triennial Network Adequacy Review,...QHP Certification and Network Adequacy Review TimelineWho doesn’t love a good calendar? We know we do. Whether you’re deep into network adequacy updates or juggling deadlines left and right, we’ve got your back. Our handy calendar...Quest Analytics® Announces Strategic Integration Partnership with Motive Practicing WiselyOVERLAND PARK, KS, April 9, 2024 – Quest Analytics, LLC, the leader in provider network compliance and performance solutions, announced today a new integration partnership with Motive Practicing Wisely, the...The Hidden Costs of Not Having Accurate Provider Data & How to Solve ItYou’ve probably heard the buzz surrounding provider data accuracy, and you might be wondering just how important it is for your organization. Well, you’re not alone! We conducted a study...Understanding CMS Exception Requests for Network AdequacyRaise your hand if you’ve ever had difficulties meeting network adequacy criteria. Well, you’re not alone. Submitting an exception request for network adequacy involves multiple components, and we’re here to...